The Burning Within: A Fight for Life After Acid Ingestion
1) Diagnosis
Primary Diagnosis : Severe corrosive gastric injury (acid poisoning) with fundic necrosis and probable gastric perforation.Secondary / Complicating Conditions :
Hypovolemic + distributive shock
Severe metabolic acidosis
Acute kidney injury (oliguria)
Severe anemia (Hb 3.1 g/dL)
Generalized anasarca and pleural effusion
Post-acid ingestion status s/p Jejunostomy (Day 3)
2) History of Present Illness (HPI)
18-year-old female was brought to the ER after intentional acid ingestion (unknown quantity). She was unconscious, unresponsive, with rapid breathing, weak pulse, and cold extremities. There was no history of trauma, fever, or seizure before ingestion. No hematemesis reported by relatives, but acid smell noted around the mouth.Negative history : No diabetes, hypertension, or drug overdose.
3) Past Medical History
No known chronic illness (HTN/DM/CAD/CKD).
No previous surgeries or ICU admissions.
No drug allergies or regular medications.
4) Physical Examination
General : Pale, cold, clammy; unresponsive (GCS E1 Vt M1); severe distress.CVS : Tachycardic, weak thready pulse, severe hypotension.RS : Tachypneic, clear initially; bilateral basal crepts later due to effusion.CNS : Unresponsive but pupils equal/reactive.Abdomen : Tender, rigid later; distension developed on Day 2.Extremities : Cold peripheries, mild edema by Day 2.
5) Vitals on Admission
HR 138 bpm
BP 60/30 mmHg
RR 38/min
Temp 98.4 °F
SpO₂ 86% on room air
GCS E1 Vt M1
6) Echocardiography (ECHO)
LV normal size, EF ~ 55%.
No RWMA.
Valves normal.
No pericardial effusion.
Shock likely non-cardiogenic (distributive/hypovolemic).
7) Investigations
Test Result Interpretation Hb 3.1 g/dL Severe anemia, probable GI bleed WBC 12 000/mm³ Stress leukocytosis Platelets 200 000/mm³ Normal Urea/Cr 70/2.1 mg/dL AKI (pre-renal) Na/K 140/3.4 mEq/L Mild hypokalemia LFT Normal — ABG pH 6.95, HCO₃ 7 Severe metabolic acidosis INR 1.8 Coagulopathy Lactate 6.5 mmol/L Poor perfusion
Follow-up Trends:
Day Na K Cr ABG(pH) Lactate 0 140 3.4 2.1 6.95 6.5 1 142 3.7 2.0 7.15 4.2 3 138 4.0 1.6 7.30 2.8
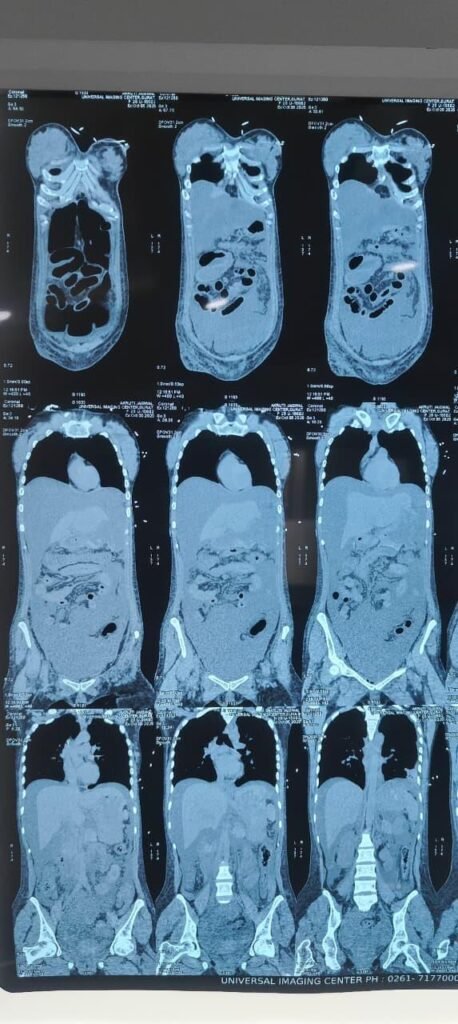
8) Imaging
CT Abdomen (5 Oct 2025, Universal Hospital)
Ill-defined, sloughed stomach wall, mainly fundus → perforation suspected.
Pneumoperitoneum, severe ascites, mesenteric haziness.
Long-segment edema in proximal small bowel + mild colonic wall thickening.
Moderate bilateral pleural effusion with basal collapse.
Generalized anasarca.
Impression: Severe corrosive gastritis with fundic necrosis ± perforation.
9) ECG & RBS
ECG : Sinus tachycardia, no ischemic changes.RBS : 110 mg/dL.
10) Day by Day Management
Day 0 – Emergency Admission to ICU
Presentation: Unconscious, unresponsive, shallow breathing, hypotension (BP 60/30 mmHg), HR 146/min, RR 36/min, SpO₂ 82% RA, Temp 99°F, GCS E1 Vt M1
ABG: pH 6.98 / HCO₃⁻ 8 / pCO₂ 24 / PaO₂ 72 → Severe metabolic acidosis
Hb 3.1 g/dL, Lactate > 6 mmol/L
Airway & Ventilation
Emergency intubation (ET 7.0 fixed at 20 cm)
Mechanical ventilation: SIMV mode, FiO₂ 100%, TV 6 mL/kg, PEEP 5 cm H₂O
Sedation: Midazolam 2 mg/h + Fentanyl 50 µg/h (for ventilator synchrony and pain control)
Circulation
2 wide-bore IV lines + central line (RIJ)
Crystalloid bolus 2 L NS, followed by maintenance 200 mL/h
Norepinephrine 0.2 µg/kg/min, titrated to MAP > 65 mmHg
Vasopressin 0.03 U/min adjunct
4 units PCV + 6 units FFP transfused → target Hb > 8 g/dL
Investigations ordered
CBC, RFT, LFT, Coagulation profile, ABG every 4 h, Trop-I, Serum electrolytes, ECG, Urine output monitoring.
Output: Urine 5 mL/h → Oliguria due to shock & renal hypoperfusion → Added Furosemide 40 mg IV stat, poor response → continued fluid and vasopressors.
Medications initiated
Drug Dose Rationale IV Ceftriaxone 2 g OD Broad spectrum coverage Pantoprazole 200 mg IV infusion@4ml/hr Stress ulcer prophylaxis / acid control Ondansetron 4 mg IV TDS Prevent retching / aspiration NaHCO₃ 20 mEq IV slow × 2 then infusion Severe metabolic acidosis Mucomix (N-acetylcysteine) infusion Mucolytic & antioxidant effect on GI mucosa Inj Tranexamic acid 500 mg TDS For upper GI mucosal bleeding risk
Day 1
Vitals : BP 82/50 (MAP 62), HR 128, RR 24 (ventilated), SpO₂ 94% on FiO₂ 60%Urine Output : 15 mL/hABG : pH 7.12, HCO₃⁻ 12, Lactate 4.2 mmol/L (Improving)Hb 8.1 g/dL, Cr 1.8 mg/dL
Changes / Additions
Continued noradrenaline 0.18 µg/kg/min, vasopressin 0.02 U/min
NaHCO₃ infusion slowed as pH > 7.1
IV Metronidazole 500 mg TDS added → anaerobic coverage
IV Albumin 20% 100 mL OD for hypoproteinemia and oncotic support
Urine output target > 0.5 mL/kg/h — started low-dose dopamine 2 µg/kg/min for renal perfusion
Investigations:
Test Day 0 Day 1 Hb (g/dL) 3.1 8.1 WBC (/mm³) 11000 14200 Plt (/mm³) 190000 165000 Cr (mg/dL) 1.2 1.8 Na⁺ (mEq/L) 138 134 K⁺ (mEq/L) 4.2 4.8 Lactate (mmol/L) >6 4.2
Day 2
Vitals : BP 98/60, HR 110, SpO₂ 96% FiO₂ 40%, Temp 99.5°FUrine output : 30 mL/h (Improving)ABG : pH 7.28 / HCO₃⁻ 18 / pCO₂ 32Labs : Cr 1.5 mg/dL, WBC 15 000CT Abdomen (Plain – Reported 5 Oct 2025):
Stomach wall ill-defined and sloughed off (mainly fundus & greater curvature) → suggestive of perforation / gangrenous gastritis
Severe ascites with pneumo-peritoneum
Left > Right pleural effusion with basal collapse
Long segment edematous small bowel wall thickening, mild colonic thickening, generalized anasarca
Interpretation :
Severe corrosive gastric necrosis with perforation and peritonitis → Surgical intervention required.
Plan:
Continue ventilatory and vasopressor support
Start Meropenem 1 g TDS IV + Fluconazole 100 mg IV OD (antifungal coverage)
Shift for surgical exploration and Jejunostomy planning once hemodynamically stable.
NPO, Ryle’s tube for drainage, monitor gastric aspirate.
Day 3 – Jejunostomy Surgery
Pre-op :
Patient on FiO₂ 40%, PEEP 5, MAP > 65 on norad 0.12 µg/kg/min
Urine output adequate, lactate 3 mmol/L
Surgery consent taken, high-risk explained
Intra-op Findings:
Extensive necrosis of stomach wall with slough and perforation at fundus/body junction.
Peritoneal soiling with acidic fluid.
Jejunostomy feeding tube placed (distal jejunum) + peritoneal lavage.
Nasogastric tube left in situ for drainage.
Post-op ICU Management:
Ventilatory support continued SIMV FiO₂ 40%
Sedation: Midazolam 1 mg/h + Fentanyl 40 µg/h
Antibiotics: Meropenem + Fluconazole continued
Vasopressors weaned over next 12 h
Enteral feeding via Jejunostomy started @ 10 mL/h after 24 h
ABG: pH 7.36 / HCO₃⁻ 21 / Lactate 2.4 → near normalization
Day 4–5 (Recovery Phase)
Extubated to O₂ via HFNC FiO₂ 35%
Norad off > 24 h
Jejunostomy feeds advanced to 30 mL/h
Urine output maintained > 0.7 mL/kg/h
CRP down from 188 → 72 mg/L
Hematocrit stable, Renal function normalized
11) Pathophysiology (Specific to Acid Poisoning with Shock and Gastric Necrosis)
Mechanism of Acid Injury
Corrosive acids (e.g., hydrochloric, sulfuric, nitric) have low pH (<2) and cause coagulative necrosis.
The hydrogen ions denature proteins, precipitate structural proteins, and create an eschar (coagulum) that may initially limit deeper penetration.
However, in high concentrations, continued proton diffusion and heat generation lead to deep transmural necrosis and perforation, especially in the stomach.
GI Tract Injury Pattern
Site Mechanism Result Oropharynx & Esophagus Rapid contact, superficial burns (if swallowed quickly) Odynophagia, dysphagia Stomach (Fundus & Body) Pooling of acid → prolonged contact + high concentration Transmural necrosis, perforation, and hemorrhage Small Intestine (Proximal loops) Secondary injury from acid spill during vomiting or perforation Edematous wall thickening and serositis (as seen on CT)
Systemic Absorption and Metabolic Effects
Metabolic Acidosis
Caused by systemic absorption of hydrogen ions and tissue hypoperfusion.
In this case, ABG pH 6.98, HCO₃⁻ 8 mEq/L, Lactate > 6 mmol/L, confirming combined metabolic acidosis (acid load + lactic acidosis from shock).
Hemorrhagic Shock
Massive mucosal bleeding from gastric necrosis → Hb 3.1 g/dL.
Severe hypovolemia → ↓ preload → ↓ cardiac output → hypotension (60/30 mmHg) → catecholamine surge, tissue hypoxia, further lactic acid accumulation.
Distributive Component (Toxic Shock) Renal Hypoperfusion → AKI
Hypotension and myoglobin/heme pigment load → acute tubular necrosis.
Manifested as oliguria (5 mL/h) and ↑creatinine (1.8 mg/dL on Day 1).
Local to Systemic Transition
Stage Local Pathology Systemic Response Stage 1 (Chemical Burn) Coagulative necrosis of mucosa, eschar formation Nausea, hematemesis, pain Stage 2 (Tissue Penetration) Sloughing, vascular thrombosis, perforation Sepsis, peritonitis Stage 3 (Systemic Decompensation) Bacteremia, cytokine storm SIRS → MODS → Shock Stage 4 (Repair/Stricture) Fibrosis during healing Gastric outlet obstruct
Why This Patient Deteriorated Rapidly
Large-volume acid ingestion → deeper gastric burn → rapid perforation and hemoperitoneum.
Delayed gastric emptying worsened contact time at the fundus and greater curvature.
Massive GI bleed dropped Hb → hypoxia-driven lactic acidosis.
Severe metabolic acidosis reduced cardiac contractility, amplifying hypotension.
Cytokine storm + vasoplegia made shock refractory → need for noradrenaline + vasopressin.
Rationale for Jejunostomy
After gastric perforation, enteral nutrition via stomach becomes impossible.
Jejunostomy bypasses injured stomach, providing early enteral feeding, preventing catabolic state, improving gut barrier integrity, and reducing infection risk.
It also allows the stomach to remain NPO for healing and drainage.
Sequential Organ Impact in This Case
Organ/System Pathophysiologic Mechanism Clinical/Lab Evidence Gastrointestinal Acid-induced coagulative necrosis → perforation CT: gastric sloughing, pneumoperitoneum Cardiovascular Hypovolemia + vasoplegia→ shock BP 60/30, tachycardia Renal Ischemic ATN from shock Oliguria, Cr ↑ to 1.8 mg/dL Respiratory Aspiration + pleural effusion CT: mild–mod effusions Hematologic Massive upper GI bleed Hb 3.1 → 4 PCV + 6 FFP transfused Metabolic Lactic + hydrogen ion acidosis pH 6.98, HCO₃⁻ 8, Lactate > 6
12) Discharge Medicines (once stabilized, post-ICU)
Pantoprazole 40 mg OD – acid suppression.
Sucralfate syrup TDS – mucosal protection.
Ceftriaxone 1 g IV BD (5 days) – infection prophylaxis.
Ranitidine via FJ (step-down).
Multivitamins + Protein supplement (via FJ).
13) Key Notes / Clinical Pearls
Always secure airway early in corrosive ingestion.
Avoid gastric lavage or induced vomiting → re-exposure risk.
CT Abdomen (plain) is diagnostic for necrosis/perforation.
Jejunostomy feeding allows nutrition while bypassing damaged stomach.
Acidosis correction + hemodynamic stability are vital for surgical timing.